- 24 X 7 Online Support [email protected]
- Contact Us +91 7520435375
- Emergency Number 0591-2411334
Migraine Headaches
What are the symptoms of a migraine?
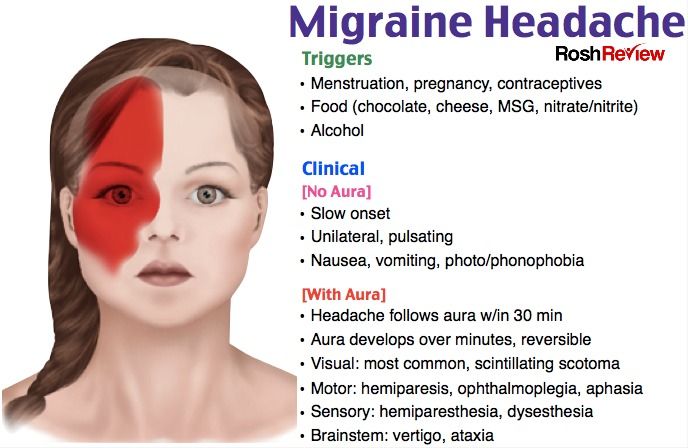
Individual migraines are moderate to severe in intensity, often characterized by a throbbing or pounding feeling. Although they are frequently one-sided, they may occur anywhere on the head, neck and face — or all over. At their worst, they are typically associated with sensitivity to light, noise and/or smells. Nausea is one of the most common symptoms and it worsens with activity, which often results in patient disability. In many respects, migraines are much like alcohol-related hangovers.
Migraine pain can be felt in the face, where it may be mistaken for sinus headache — or in the neck, where it may be mistaken for arthritis or muscle spasm. Complicating the diagnosis of migraine is that the headaches may be accompanied by other "sinus like" symptoms, including watering eyes, nasal congestion and a sense of facial pressure. Most patients who think they have sinus headache in fact have migraines.
In up to 25 percent of patients, the migraine headache pain may be preceded by an aura, a temporary neurological syndrome that slowly progresses and then typically resolves just as the pain begins. While the most common type of migraine aura involves visual disturbances (flashing lights, zigzags, blind spots), many people experience numbness, confusion, trouble speaking, vertigo (spinning dizziness) and other strokelike neurological symptoms. Some patients may experience auras without headaches.
Migraines are about three times more common in women than men, and may affect more than 12 percent of the U.S. adult population. Migraines often run in families, and can start as early as elementary school but most often in early adulthood. They often fade away later in life, but can strike at any time. The most common cause of recurring, disabling headache pain, migraines are also the most common underlying cause of disabling chronic, daily headache pain. While migraines are the No. 1 reason that patients see a neurologist, most cases are handled by primary care physicians.
Things that can make the headaches more likely to occur include:
- Alcohol
- Weather changes
- Lack of sleep
- Schedule changes
- Dehydration
- Hunger
- Certain foods
- Strong smells
- Teeth grinding at night
- Menstruation
Despite their dramatic symptoms, migraines are almost never due to an underlying problem that will show up on any testing, even on brain MRIs. Many experts do not recommend brain imaging at all, even in severe cases, as long as the patient's symptoms are typical for migraines and a thorough neurological examination is normal.
There are extremely rare families that have migraines as a result of a single genetic mutation in one of four known genes that can lead to the condition called familial hemiplegic migraine. There are no genetic tests for the vast majority of patients. Because the condition cannot be diagnosed by scan or blood test, the diagnosis is "clinical" — made by an experienced physician.
Migraines that are severe, frequent or accompanied by neurological symptoms are best treated preventively, usually with a combination of dietary modification, lifestyle changes, vitamins and daily prescription medications. Most of our best preventive medications are often used for other medical purposes as well; the majority are blood pressure drugs, antidepressants or epilepsy medications. Individual headache attacks are best treated early, often with one or more of the following types of medications: triptans, nonsteroidal anti-inflammatory drugs (NSAIDs), anti-emetics (anti-nausea), and sometimes narcotics or steroids.
Migraines typically last a few hours to a couple of days and respond well to specific treatments. However, in some patients, the migraine is particularly severe and long-lasting — and may even become chronic, occurring continuously for weeks, months or even years. If improperly managed or left untreated, intermittent migraines may essentially transform into a chronic daily headache, with continuous and smoldering symptoms that periodically erupt into a "full-blown" migraine. This condition is extremely difficult to treat.
Other patients may develop increasingly frequent headaches as a result of overusing their short-acting headache medications. See medication overuse headache. While they are considered primary headaches, meaning they have no known underlying cause, migraines are associated with an increased risk of stroke, brain scarring as seen on MRI scans, a heart defect called a patent foramen ovale (PFO) and other medical conditions.
At the Johns Hopkins Headache Center, located at the Johns Hopkins Bayview Medical center, we have expert physical therapists, nutritionists and psychologists who work closely with our neurologists to help manage patients with frequent migraines. Biofeedback and relaxation techniques are available to complement our standard medical treatments.



